Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PMJAY) 2023
Introduction
Features of PMJAY
-
PM-JAY is the world's largest government-funded assurance/health insurance scheme. All applicants who have enrolled in the scheme will be able to obtain a medical insurance scheme worth INR 5 lakhs. This sum is for one fiscal year.
-
People living in both rural and urban areas will be able to enrol in this scheme if they meet the other eligibility criteria. Beneficiaries from villages and urban settlements have been identified in proportions of 85% and 60%, respectively. Only patients admitted to empanelled hospitals will be able to receive cashless and paperless treatment.
-
The scheme will be implemented throughout the country. The central government has highlighted some implementation methods for ease of operation. Each state will be able to select the mode of implementation that best suits its needs.
-
It pays for up to three days of the period before hospitalization and up to fifteen days after hospitalization expenses, for example, medications and diagnostics.
-
This sum is meant to cover all secondary and most tertiary care expenses.
-
There are no restrictions on the age, size, or gender of the family.
-
Already existing conditions are covered from the start.
-
A three-tier model is used to implement the scheme throughout the country.
-
The AB-PMJAY is implemented by the National Health Authority throughout the country. The SHAs or the State Health Agencies have been established to ensure the effective implementation of AB-PMJAY at the state/territorial level.
-
District Implementation Units, or DIUs, have been established to ensure on-the-ground coordination among scheme stakeholders and smooth implementation.
Eligibility
Rural Communities
-
Landless households whose primary source of income is manual casual labour
-
Families with no adult members aged 16 to 59
-
Households of SC/ST
-
Families with only one room and Kucha walls and roofFemale-headed households with no adult male member aged 16 to 59
Families in rural areas with one or more of the following characteristics: households without shelter, homeless, living on charity, manual scavenger families, primitive tribal groups, and legally released bonded labour.
For Metropolitan Areas
-
Domestic helper
-
Sweeper, maali, tailor, sanitation worker
-
Beggar
-
Street vendors, hawkers, or any other service provider who works on the streets
-
Ragpicker
-
Plumber, welder, labourer, construction worker, security guard, painter, mason, and other jobs
-
Driver, transport employee, conductor, a rickshaw puller, cart puller
-
Mechanic, repairman, electrician, and assembler
-
Washerman , chowkidar
-
Peon in a small establishment, delivery boy, shop employee, waiter, attendant, assistant
Exclusions
-
Families who pay income tax or professional tax
-
Households with a Kisan card with a credit limit greater than INR 50000.
-
Any member of the family whose earnings are greater than INR 10000 per month
-
Government employee
-
Households with non-agricultural enterprises that have been registered with the government
-
Any member who possesses over 2.5 acres of irrigated land and 1 piece of irrigation equipment or owns 5 acres or more of irrigated land for at least two crop seasons or has at least 7.5 acres of land and at least one irrigation system
-
Families who own a motorized wheeler or fishing boat
Hospitalization Under the Ayushman Bharat Scheme
Diseases Covered in PMJAY
-
Surgery of skull
-
Prostrate cancer
-
Pulmonary valve replacement
-
Fixation of the anterior spine
-
Replacement of double valve
-
Gastric pull-up with laryngopharyngectomy
-
Bypass surgery of coronary artery
-
Carotid angioplasty with stent
Diseases Not Covered In PMJAY
-
Transplant of organs
-
Procedure related to cosmetics
-
OPD
-
Drug rehabilitation program
-
Any procedure related to fertility
-
Diagnostics for evaluation of individuals
Expenses or Services Covered under the Scheme
-
Services for Intensive and Non-Intensive Care
-
Pre Hospitalization expenses
-
Lab Investigation and Diagnosis
-
Medicines and medical consumables
-
Expenses related to treatment, medical examination, and consultation
-
Post Hospitalization expenses for the next 15 days after hospitalization
-
Treatment and testing for Covid-19
-
Food-related services
-
Complications that arise during treatment
-
Benefit of accommodation
Difficulties in Adopting PMJAY
Cooperation of States:
The Cost Burden:
Unnecessary Treatment:
Inadequate Health Resources:
How to Get Yourself Enrolled in the PMJAY Scheme?
-
Contact Details
-
Certificate of identification and age
-
Income Proof
-
Caste Certificate
-
Document for current family status
Procedure to File a Claim Under PMJAY
-
You must identify the accredited hospitals that provide PMJAY treatment. Admit yourself to the hospital and present your PMJAY health card as identification.
-
After some paperwork was completed to verify the insured's identity, treatments would be permitted on a cashless basis.
-
You would not have to pay for your own medical expenses because the scheme would cover them.
How to Get Your Ayushman Card Online
-
Go to PMJAY's official website and fill in your personal information.
-
Enter your Aadhaar card number and select approve beneficiary
-
Now, enter the password and pin number into the CSC wallet.
-
It will take you to the website's home page.
-
The download option is visible. Place it in front of your golden card and click on it.
-
The Ayushman card has been downloaded.
Benefits of the PMJAY Scheme
-
The Pradhan Mantri Jan Arogya Yojana card holder is entitled to a number of perks. Beneficiaries from the weaker parts of society can have access to high-quality healthcare without facing too many financial troubles as a result of unintended or long-term vital medical procedures.
-
Standard mediclaim coverage excludes pre-existing ailments, internal congenital disorders, and mental health issues.A solid IT foundation underpins the system-
IT assists with beneficiary identification, the maintenance of treatment records, the processing of claims, the resolution of grievances, and so on.
Both the national and state levels have a fraud detection, prevention, and control system, which is crucial for combating fraud. -
The initiative has the potential to spark major changes in India's healthcare sector.
-
The system compels hospitals to meet a specific level.
-
Insurers and third-party administrators will have access to the vast new market created by the plan.
Achievements of the PMJAY Scheme
Frequently Asked Questions
What is the coverage under Pradhan Mantri Jan Arogya Yojana?
Which type of medical or healthcare services are not covered under the Pradhan Mantri Jan Arogya Yojana?
Which was the campaign under which the Pradhan Mantri Jan Arogya Yojana was launched?
What are the documents required for applying to get enrolled in the PMJAY Scheme?
-
Contact Details
-
Certificate of identification and age
-
Income Proof
-
Caste Certificate
-
Document for current family status
What are the different expenses or services that are covered under the scheme?
Can hospitals charge beneficiaries money for treatment under PMJAY?
Are there any diseases that are not covered by the scheme?
What are the minimum and maximum ages for participation in the PMJAY scheme?
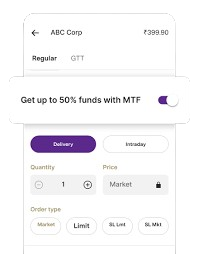
Never miss a trading opportunity with Margin Trading Facility
Enjoy 2X leverage on over 900+ stocks